Interventional Care


We notice that you are visiting us from . This site only services US-based visitors. Would you like to visit the site that is appropriate for your location?
Did you know that one in ten persons who contract the Legionnaires disease will die from it? (1). Although it’s rare that we would even think of Legionnaires; When it rears its ugly head the results can be disastrous for those who are exposed.
Exposing its Identity:
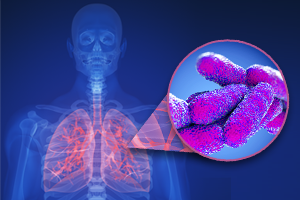
Legionnaires’ disease (Legionella) is a type of pneumonia that is caused by inhalation of aerosolized water containing L pneumophila bacteria. Legionnaires’ disease cannot be contracted through person to person contact, but rather must be inhaled through the lungs from contaminated droplets of water. This particular type of bacteria can grow quickly under certain circumstances and if aerosolized the bacteria can pose a great risk to human health. The bacteria also can cause Pontiac fever, a milder form of the disease which most often resembles the flu. The two diseases together are called legionellosis. Prompt treatment with antibiotics will usually clear and cure the disease.
Uncovering its Hideout:
When thinking about Legionella most people think water cooling towers and central water heating systems. Recently, New York City dealt with an outbreak situation linked to water cooling towers (3), following a massive 138 recorded cases in 2015. And, in November, 15 cases of Legionnaires disease were confirmed in Disneyland in Anaheim, CA (the source has yet to be found (2)).
The truth is that the risk of Legionella can lurk in the unlikeliest and most innocuous of places. In January, 2012 Washington Post published “Hospital Fountain Linked to Legionnaires Outbreak” where eight people contracted Legionnaires after passing by or sitting near a decorative water wall in the entry of a hospital in Wisconsin (4). None of them were patients in the hospital at the time they contracted the disease. They were simply visitors or delivery personnel.
Legionella can colonize and grow anywhere that water is present and growth parameters are met. Drinking fountains, water coolers, ice dispensers, dental water lines, pools and hot tubs, spa facilities and shower areas can be potential culprits linked to legionella (5) (6).
What few people realize is that complete eradication of legionella in plumbing systems and drinking water is very unlikely, because it is naturally occurring in the outdoor environment (7). Despite a utility company’s best attempts at disinfection, low numbers of the organism may still enter buildings from public water sources, colonizing pipes and water reservoirs (8).
What is the KEY to preventing Legionnaires disease? Prevention of colonization and growth of bacteria ANYWHERE water is used or stored remains key.
For prevention of Legionella in the water distribution system, the CDC recommends maintaining hot and cold water temperatures as mandated by state law. For the most up to date recommendations for healthcare facilities, the CDC also refers to the ASHRAE (American Society of Heating, Refrigeration, and Air-Conditioning Engineers) standard called “ASHRAE 188-2015”. ASHRAE water temperature recommendations for Legionella control are as follows: hot water heater outlet temperature at or above 60°C (140°F); hot water temperature at coldest point in hot water heater, storage tank or distribution system at or above 51°C (124°F); cold water temperature in any part of system at or below 25°C (77°F). If it is determined that these temperatures cannot be achieved, then additional hazard control measures are required.
For Chlorine concentrations; chlorine concentration recommendation for Legionella control is >0.5 ppm (mg/l) free residual oxidant, as chlorine. Again, if this cannot be met then additional supplemental treatments may be required (9). The CDC also recommends either periodic increases to >150°F or chlorination with flush (1). Other approaches have also been used such as copper-silver ionization or chlorine dioxide, however it is important to insure the materials are EPA approved for the application and levels are maintained within safe drinking water limits. Regardless of the treatment method selected, the facility should establish validation procedures to assure adequate biological control. Routine testing for the bacteria should also be a part of a prevention and water maintenance program.
Unfortunately, this naturally occurring environmental pathogen is not going away anytime soon, and healthcare administrators need to be constantly alert to possible reservoirs where Legionella can grow, and stay vigilant with adhering to water system cleaning and maintenance.
Effective Environmental Programs
Prevention of disease in facilities is an ongoing battle and the bedrock of any infection control and prevention program must include a comprehensive approach. Legionella prevention steps must be incorporated into a well-established environmental disinfection program. A robust program is key in preventing routine transmission of disease and mitigation of potential outbreak situations. This core program should include:
Though hearing about interesting organisms, such as Legionella, and the infections that they cause makes for lively conversation, the emphasis is always on patient and public safety. By adhering to recommended protocols outlined by CDC and ASHRAE, people may enjoy the pleasantries in life (spas, water fountains, Disneyland) and less pleasant but sometimes necessary stays within healthcare without worry.
1 (CDC https://www.cdc.gov/legionella/fastfacts.html)
2 http://www.ocregister.com/2017/11/15/3-more-cases-of-legionnaires-disease-confirmed-in-outbreak-linked-to-anaheim-and-disneyland/
3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5652439/
4 https://www.washingtonpost.com/national/health-science/hospital-fountain-linked-to-legionnaires-outbreak/2012/01/10/gIQAyLwEpP_story.html? utm_term=.0d3d72a46004
5 Cabot AL, Miller RL, Micik RE, Ryge G. Studies on dental aerobiology: IV. Bacterial contamination of water delivered by dental units. J Dent Res 1971; 50(6):1567-1569
6 Atlas RM, Williams JF, Huntingdon MK. Legionella contamination of dental unit waters. Appl Environ Microbiol 1995;61:1208-1213
7 ASHRAE Technology Council. Position Document on Legionellosis. Approved, June 25, 1998; Reaffirmed January 25, 2012.
8 US EPA. Water utility companies in the US treat almost 34 billion gallons of water every day. In the US and Canada, approximately one million miles of pipes or other constructed conveyance (enough to circle the globe 40 times) carry water to consumers. epa.gov.
9 https://www.ashrae.org/standards-research–technology/standards–guidelines/guidance-on-reducing-the-risk-of-legionella