Interventional Care


We notice that you are visiting us from . This site only services US-based visitors. Would you like to visit the site that is appropriate for your location?
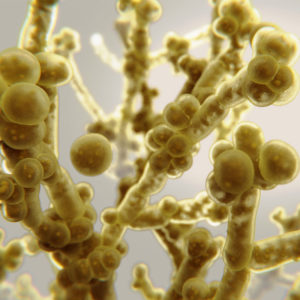
Candida auris is a newly emerged fungal pathogen that is often resistant to antifungal drugs. It is a serious global health threat and has caused severe infections with high mortality in many. As the total amount of Candida auris cases continue to rise in the United States, healthcare facilities and hospitals are learning what measures need to be taken in order to improve their response to the aggressive and naturally resistant fungus. This Q&A is intended to address some of the common questions about C. auris.
Testing has shown that Candida auris can survive for weeks on surfaces1. More specifically, studies have shown that C. auris can persist on surfaces in the healthcare environment for at least 14 days (Piedrahita et al., 20172; Welsh et al., 20173); C. auris has been cultured from contaminated bedding for up to 7 days (Biswal et al., 2017)4.
Candida auris is a newly emerged fungal pathogen that presents a global health threat as the organism is often resistant to multiple anti-fungal therapies used to treat infection and it is difficult to identify with standard laboratory methods which often leads to misidentification and improper management. This can result in silent transmission within healthcare and nursing home settings resulting in outbreaks1. Mortality is high following infection, 30-60% of those with C. auris infection have died1.
Candida auris can cause bloodstream and other types of invasive infections, particularly in hospitalized patients, and in nursing home residents who have multiple medical problems1.
People who have recently resided in a nursing home and have indwelling devices (such as breathing tubes, feeding tubes, and central venous catheters) are at the highest risk of infection with C. auris. Also, those who have had recent surgery, diabetes, a broad-spectrum antibiotic, and anti-fungal treatments are at risk. Infections have impacted those of all ages, and much is still being learned about risk factors of infection1.
Candida auris is spread via contact with contaminated environmental surfaces or equipment and from person-to-person transmission in healthcare settings. Due to the nature of transmission, hand hygiene is a critical intervention, along with contact precautions used in healthcare facilities, and enhanced barrier precautions used in nursing homes5. Additionally, the Centers for Disease Prevention and Control (CDC) has mentioned that more work is needed to better understand how C. auris spreads1.
Candida auris has the potential to rapidly spread within the healthcare setting, especially during the pandemic due to the diversion of resources for pandemic response. To mitigate the spread of this organism, it is important to ensure that the facility’s laboratory has the testing methodology to accurately identify C. auris; if not, isolates under consideration should be sent to the state or local public health laboratory for identification. There needs to be a surveillance protocol that allows for appropriate testing of those patients/residents considered high risk for C. auris and prompt laboratory notification when C. auris is suspected in culture. Communication between facilities during the transfer of patients/residents who are suspected/confirmed to have C. auris infection/colonization is critical to halt transmission as appropriate precautions can be implemented. Finally, education is a key factor for the infection prevention and control interventions (hand hygiene, transmission-based precautions, environmental disinfection) with healthcare staff, including environmental services5.
The CDC recommends the use of an Environmental Protection Agency (EPA)–registered hospital-grade disinfectant effective against C. auris. Use a disinfectant that is effective against C. auris (EPA List P: Antimicrobial Products Registered with EPA Claims Against Candida Auris) or if these products are not available, use a product from the EPA List K for products that are effective against C. difficile5. PDI offers multiple products within their surface cleaning and disinfection portfolio that appear on the EPA’s List P and List K:
Thorough daily and terminal cleaning and disinfection of patients’/residents’ rooms, and all areas where they may receive care, should be performed using an appropriate disinfectant. Shared equipment needs to also be cleaned and disinfected before use on another patient. It is important to follow the manufacturer’s directions for use, including the application of the product for the correct contact time5.