Interventional Care


We notice that you are visiting us from . This site only services US-based visitors. Would you like to visit the site that is appropriate for your location?
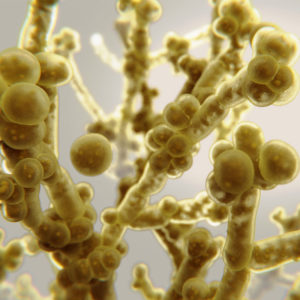
Candida auris (c. auris) appears to be taking advantage of hospitalized patients during the pandemic. As with all MDROs, colonization can quickly become infection when host immunity is compromised and/or invasive devices create an easy entry portal.
C. auris thrives in the healthcare environment as it successfully attaches to sheets, bedrails, doors, and medical devices- making it easy to colonize the skin of hospitalized patients- and transmit within the facility1. C. auris grows optimally at 37-42° Celsius (98.6-107.6°F) 2, making the human body an ideal growth site. Hospitalized COVID-19 patients often need intensive care and may require the placement of catheters (urinary, peripheral/central venous, feeding and ventilator tubing).
The catheter tubing is a prime surface for C. auris to take up residence, providing optimal entry into the body to cause infection. Chowdhary, et al reported that 50% of C. auris patients required ventilation because of severe COVID-19 pneumonia, and all patients with candidemia had indwelling central lines and urinary catheters3. This same study also found that C. auris infections were probably hospital acquired, with patients having prolonged ICU stays, as well as underlying chronic conditions.3 Interestingly, Zuo, et al reported the fecal fungal microbiome of COVID-19 patients shows an increasing prevalence for opportunistic fungal pathogens, including C. albicans, C. auris and Aspergillus flavis4. This could also impact C. auris colonization and infection rates, as well as transmission, within those hospitalized during the pandemic.
In 2020, there has been a 400% increase in confirmed cases of C. auris (compared to case numbers in 2018, the most recent year with data available).1 It would be safe to assume that cases may be much higher, as colonization often exists without infection, and the current pandemic has impeded C. auris surveillance efforts. To a certain degree, this could also be the natural progression of spread of the multi-drug resistant organism. As laboratory identification can be difficult and the use of anti-fungal therapies aren’t always tracked within stewardship programs, both could be helping drive the prevalence of this organism.
With COVID-19 cases surging now in the fall and winter months, the importance of testing and contact tracing will be critical to control the spread of newly emerging and often difficult to treat organisms1. As Borman, et al concluded, overwhelmed intensive care units (ICUs), breakdown of infection prevention measures, and high-risk patients requiring mechanical ventilation and other invasive supportive care due to the COVID-19 pandemic, appear to provide ideal conditions for outbreaks of C. auris5.
It will remain imperative that basic infection prevention measures are maintained to curtail the spread of all MDROs during this pandemic: PPE compliance (where resources allow as PPE availability is limited), hand hygiene products, like PDI Sani-Hands® wipes, environmental cleaning and disinfection (See EPA List N for SARS-CoV-2 approved products), as well as isolation precautions, appropriate use of antimicrobials, and continued surveillance of MDROs and antimicrobial resistance.
References